Overview
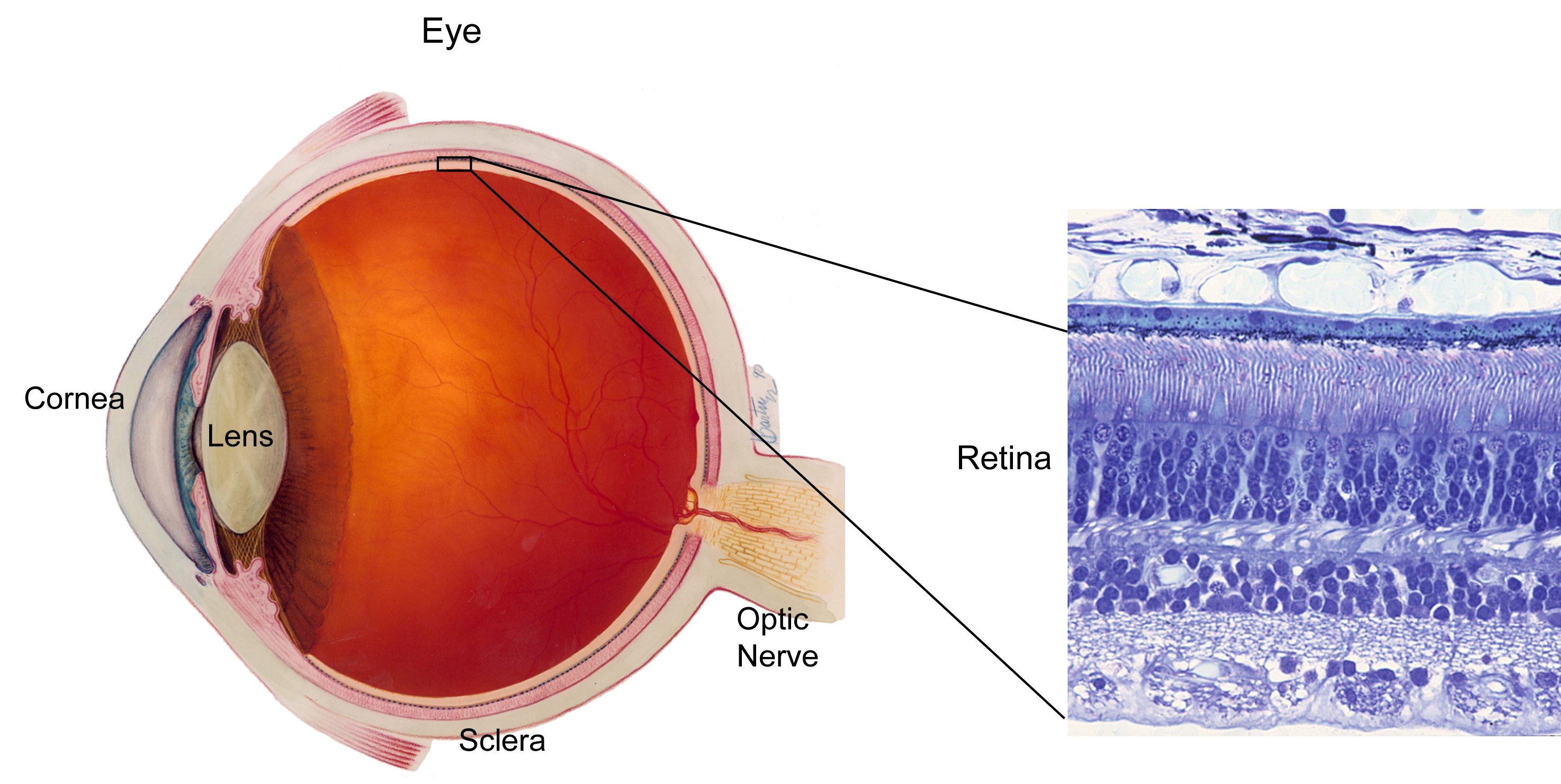
The Retina (& macula)
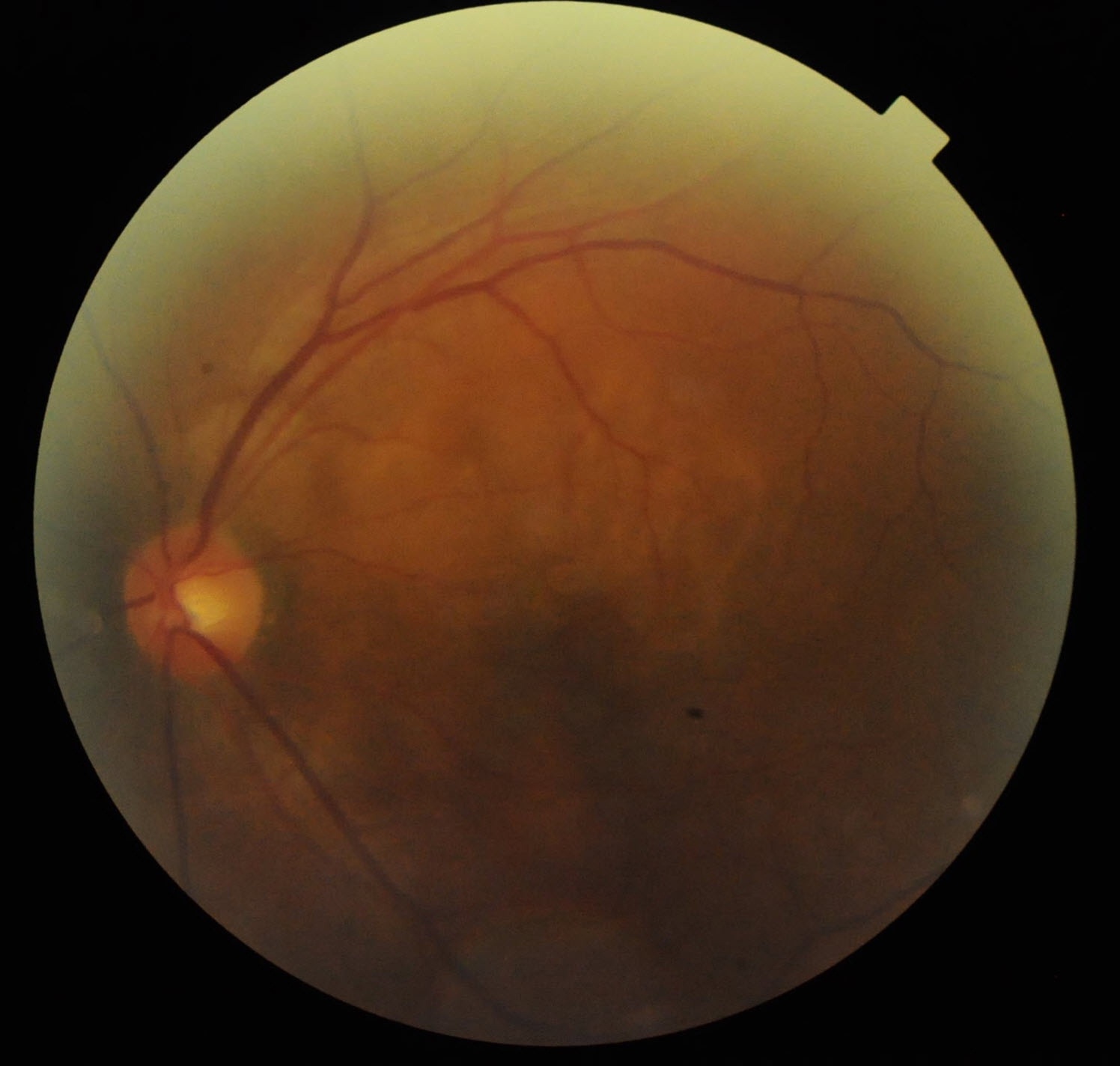
The retina is a layer of nerve tissue at the back of the eyeball, much like a film in a camera. It is light-sensitive and transmits signals to our brain via the optic nerve, where it is interpreted as images. The macula is a small area on the retina near the centre of the retina. This is the most-sensitive part of the retina and is responsible for sharp and high-resolution vision.
Complications
Floaters and Flashes
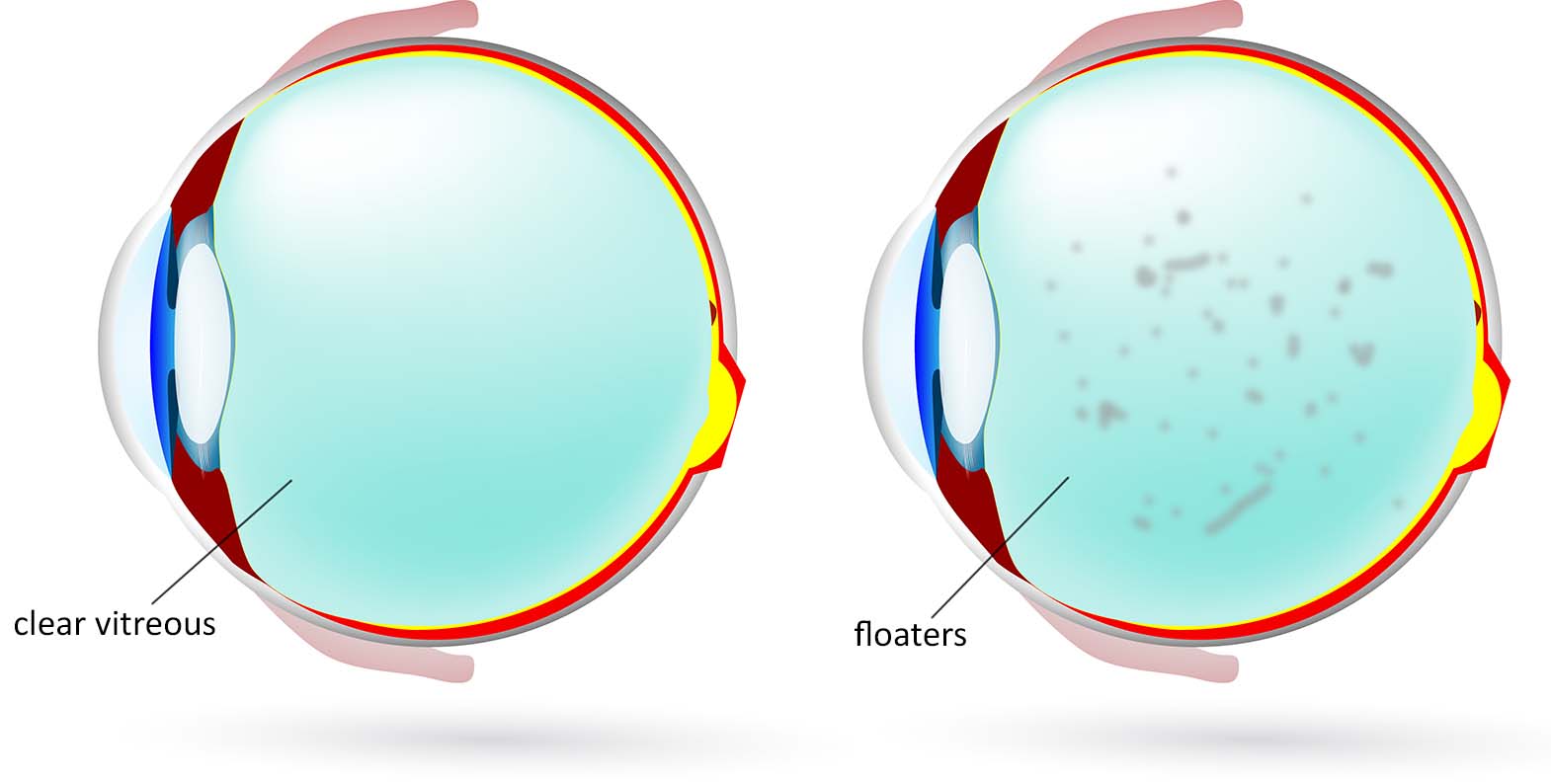
The cavity of the eyeball is filled with a gel-like substance known as the vitreous. It helps to maintain the shape of the eyeball. The vitreous contains fine collagen fibres hat is attached to the surface of the retina. As we age (and in conditions such as high myopia, or after an eye injury), the vitreous liquefies and the fibres form clumps that float in the eyeball cavity. This is known as ‘vitreous syneresis’, and the floating clumps cast a shadow on our retina that we perceive as ‘floaters’. As the vitreous gel is separating from the surface of the retina, it pulls on the retina, sending signals to the brain that we perceive as ‘flashes’. These typically occur in the corner of the vision like lightning streaks, usually more visible during dim lighting and even when the eyes are closed.

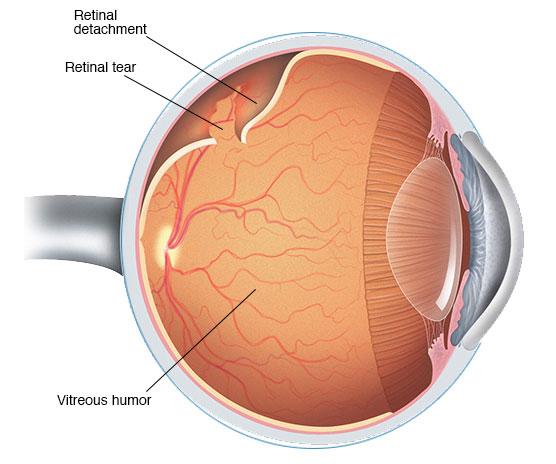
What is a retinal break (tear) and retinal detachment ? How does it occur?
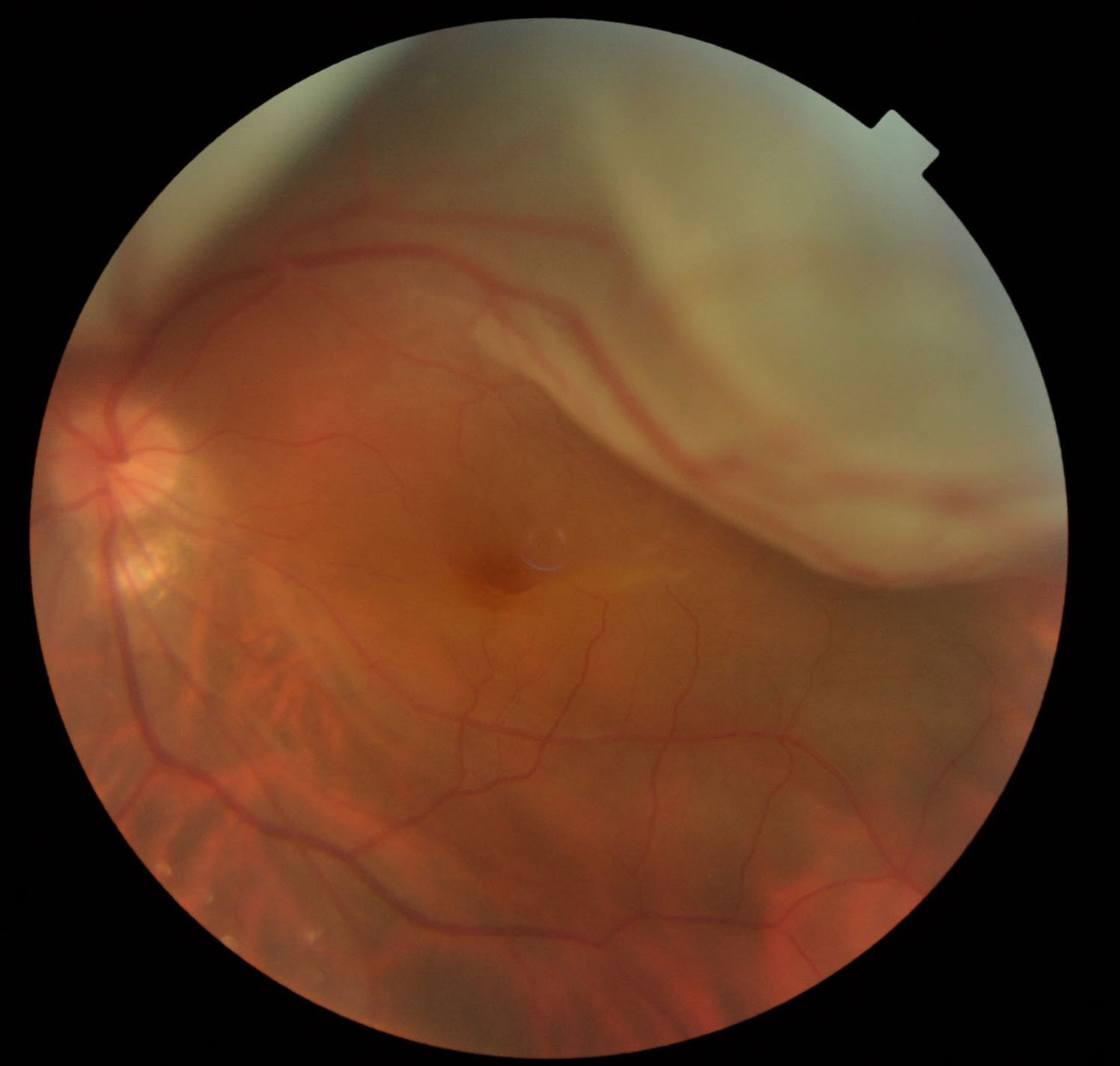
In most cases, the vitreous gel typically separates smoothly as it pulls away from the surface of the retina. However, in a few patients, the gel may be firmly attached or attached to an anatomically weakened area of the retina. In the process of pulling away, this can cause a tear on the retina. Following the tear, fluid within the eye can find its way behind the tear beneath the retina. This causes the retina to be lifted away from the wall of the eyeball. This is known as a retinal detachment which can be a sight-threatening condition
Sudden onset of flashing lights with increased floaters or hair-like objects, o the perception of a shadowy curtain covering a portion of your vision might indicate a retinal tear or detachment. You are advised to see your ophthalmologist immediately, as it has the potential to quickly lead to blindness. Book an appointment here.
Types of Retinal Detachments
Rhegmatogenous
-
-
This is the most common form of retinal detachment, and is caused by a tear or break in the retina (as described above). This allows fluid to seep under the retina separating it from the back layer of the eyeball (the retinal pigment epithelium).
-
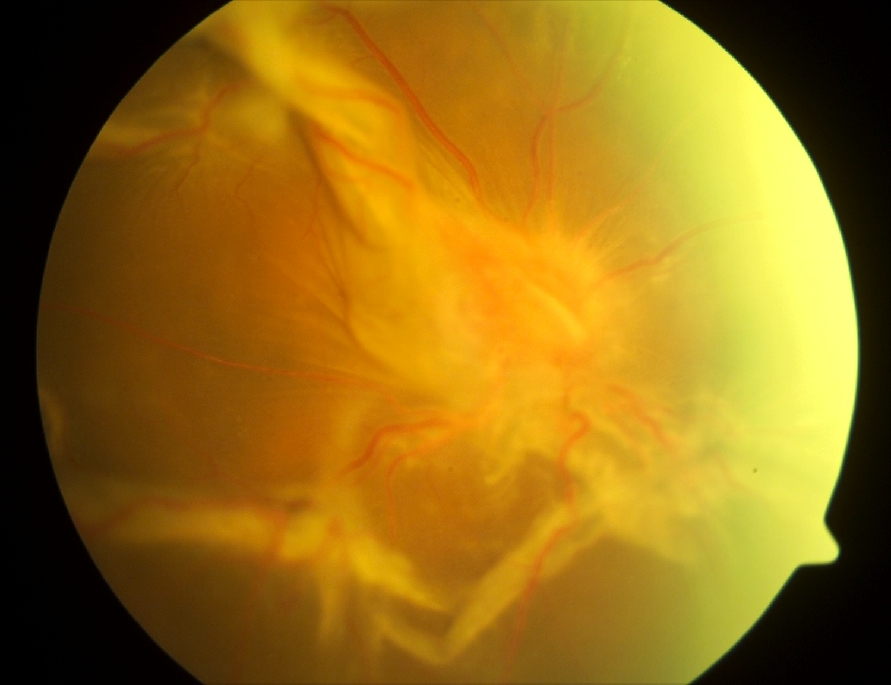
Tractional
-
-
This form of retinal detachment occurs when scar tissue caused by abnormal new vessels (neovascularization), chronic inflammation or severe injury, forms on the surface of the retina. The contraction of the scar pulls the retina away from the back of the eyeball. Tractional retinal detachment can also cause tears and holes on the retina further complicating the problem.
-
Exudative
-
-
This is an uncommon form of retinal detachment. It is caused by retinal diseases including inflammatory disorders, vascular abnormalities, tumour or trauma, where fluid accumulates beneath the retina, in the absence of a retinal tear. Surgery is NOT to be performed in this category and treatmentis often medical.
-
Symptoms
The most common visual symptoms include a sudden increase in the number of floaters accompanied by flashes of light in the peripheral part of the vision. This may progress to a dark shadow or curtain starting from the peripheral field of vision. When the macula is detached, there may be distortion and loss of central vision (blurring).

How are Retinal breaks & Retinal detachments treated?
Retinal Break & Tears
1) Laser Photocoagulation
Tiny burns (photocoagulation) are made around the retinal tear, creating a scar tissue that will wall off the retinal tear. This will prevent fluid from leaking under the retinal tear.
Laser treatment is usually performed as an outpatient procedure on a slit lamp laser machine with the aid of a lens for visualization.
2) Freeze Treatment (Cryopexy)
Cryopexy is a technique that utilizes liquid nitrogen to cause freezing around outside the retinal tear with the help of a probe. Like laser photocoagulation, it causes scarring around the retinal tear and prevents retinal detachment. A local anaesthetic is usually required to perform this procedure.

Retinal Detachment Surgery
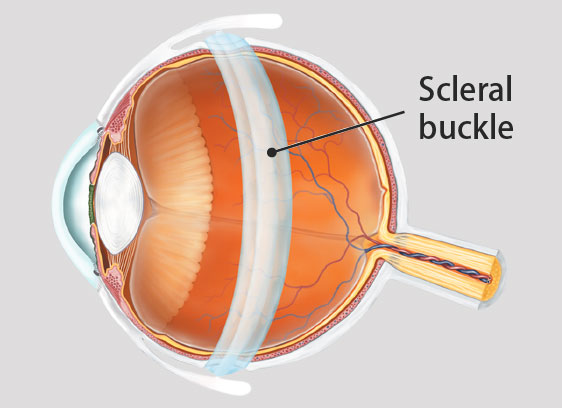
1) Scleral buckle surgery repair
This technique involves the use of a silicone band that is applied to and stitched around outside the white of the eye (the sclera). It serves to support the retinal break by pushing the wall of the eye inwards against the retinal tear, allowing reattachment of the retina. Cryotherapy is usually used to cause scarring around the tear. The fluid beneath the retina may be drained with a small puncture, or may sometimes be left to resorb on its own.
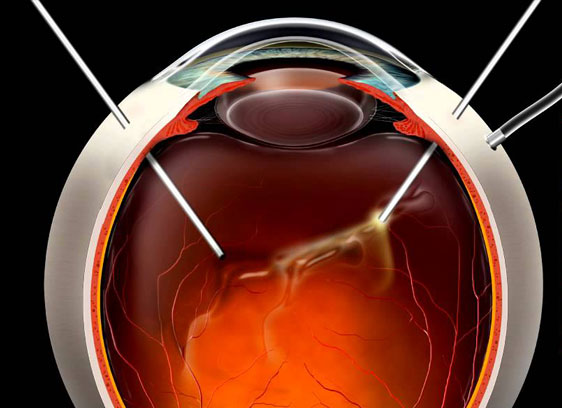
2) Vitrectomy
Vitrectomy is an intraocular procedure where tiny incisions are made through the sclera. In this technique, the vitreous is removed completely with a cutter and the subretinal fluid is sucked out, thus flattening out the detached retina. Laser photocoagulation or cryopexy is used to cause scarring around the tears. At the end of the surgery, gas or silicone oil is placed into the eye to assist in flattening out the retina. You will need to position your head (posturing) for several days to keep the gas or oil in contact with the retinal tear(s) to keep the retina attached. Over time, the gas will be resorbed on its own. However if oil is used, a second procedure will need to be performed subsequently to remove the oil. The instruments used in modern vitrectomy are typically of small diameter (23G, 25G or 27G), they do not require any sutures (sutureless surgery). Sometimes a vitrectomy is combined with a scleral buckle surgery in more complicated cases.
Outcome
Retinal detachment repair surgery that is usually a day procedure that can be performed under local or general anaesthesia. In some cases, especially complicated retinal detachments where surgical time is longer, it may be prudent to stay overnight in the hospital for observation.
The overall success rate for retinal reattachment surgeries is about 90-95%. Some cases may require 2 or more procedures. Sometimes, even under the best circumstances treatment may fail despite multiple attempts and vision may be eventually lost.
The final visual outcome may not be known till the gas resorbs or oil removed after several weeks to months. If the macula was not detached prior to surgery, good vision is usually preserved. However, if the macula was previously detached, the final visual acuity will not be as good as prior to the detachment. As such you should seek an immediate consult with your Eye Surgeon in the event of visual symptoms or floaters and flashes, as early diagnosis and intervention is paramount to preservation of good vision in cases of retinal detachment.
If you ever experience any of the above symptoms, see your Ophthalmologist immediately or go to the nearest Emergency room right away to check your eye condition. Book for an evaluation here
